Published: Australian and New Zealand Journal of Psychiatry
Authors: Professor Christopher W Lee & Dr Aaron DJ Frost
In a recent paper, Professor Jorm (2018) concluded that there was no discernible impact of the Better Access Scheme on the mental health of the Australian population. In making this conclusion, Jorm focussed on two population metrics, namely, the prevalence of psychological distress as measured by the K10 and the annual suicide rate. He argued that the increased use of mental health services after the introduction of Better Access had no detectable effect on either measure. K10 data, however, significantly varied during periods that align with changes in Better Access. Furthermore, for several reasons, the annual suicide rate is not a reasonable metric to assess the influence of Better Access on population health. While it is undoubtedly important to evaluate the Better Access initiative, that evaluation should occur in the context of the intended purposes of Better Access.
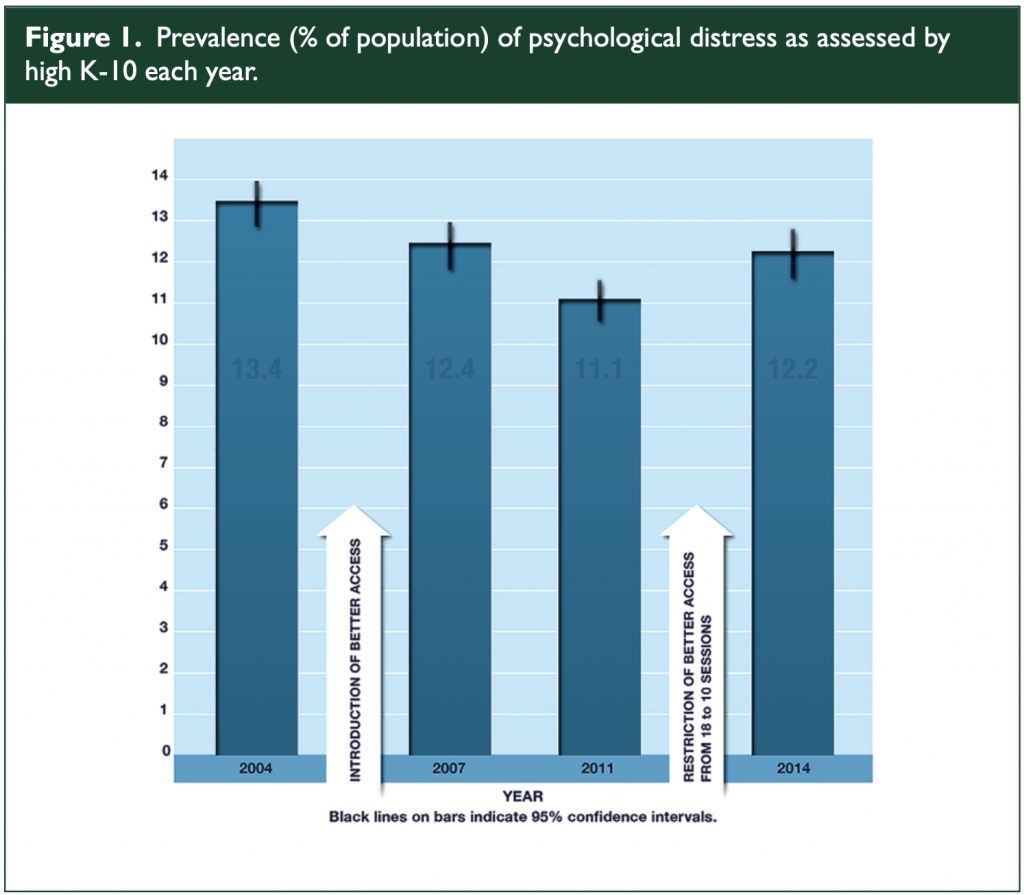
Figure 1. Prevalence (% of population) of psychological distress as assessed by high K-10 each year.
Using the same K10 population data reported by Jorm, Harvey et al. (2017) estimated the prevalence of common mental disorders with high or very high symptoms. They concluded that, while there was no significant change in very high symptom levels between 2001 and 2014, there was a significant decrease during this period for probable common mental disorders with high symptom levels (p < 0.001). K10 scores declined following the introduction of Better Access in 2006. During the next data period, when there was an increase in uptake of Better Access, mean K-10 scores declined even further. Examination of Figure 1 shows the
significance of these changes in that the confidence interval for the 2004 mean K-10 score does not overlap with the intervals for both 2011 and 2014. It is notable that the improvements were maintained after 2011, when the number of rebated sessions was reduced from 18 sessions to 10 sessions in a calendar year.
Population-level data on rates of suicide are inappropriate to measure the effectiveness of Better Access. Better Access was never designed as a suicide prevention initiative and suicide is a complex phenomenon that has multiple risk factors. The most comprehensive psychological autopsy data we have in Australia is the Queensland Suicide Register. In a 2016 report on 1914 completed suicides, only 47.2% of people who took their own life had a diagnosable mental health disorder. Given that a diagnosis is an essential requirement to activate a mental health care plan under Better Access, this suggests that over half of completed suicides would not have been eligible to be referred to Better Access. Similar findings have been reported in larger international population cross-sectional studies (Crump et al., 2014). In this Swedish study of 7 million people, 56% of the women and 39% of men who died by suicide also had a psychiatric disorder. Specific somatic disorders such as chronic obstructive pulmonary disease, cancer, spine disorders, asthma and stroke were significant independent risk factors. Of course, none of these are currently targeted in Better Access. Within psychiatric disorders, the greatest increased risk was associated with substance use disorders, psychotic disorders, depression (particularly severe forms) and personality disorders. Recent literature has shown that many of these psychiatric conditions would not have been treated with a sufficient dose if restricted to the 10 sessions rebated by Better Access. For example, 26 sessions have been found to be the optimal dose for providing
cognitive-behavioural therapy (CBT) for psychotic patients (Lincoln et al., 2016).
Finally, the stated aims of Better Access were to improve the treatment and management of mental illness within the community and also to increase community access to mental health professionals. On this second objective, the population data are unequivocal in support of the success of the programme. The population treatment rate for mental disorders in Australia increased from 37% to 46% in the first 3years of Better Access which was concluded to be most likely due to the introduction of the programme (Whiteford et al., 2014). Finally, as acknowledged by Jorm, the data from the formal evaluation to date indicate that Better Access has resulted in substantial symptom improvement for those people engaged in the programme. However, the methodology of this evaluation could be improved and further research in this area would be welcomed.
Declaration of Conflicting Interests
A.D.J.F. and C.W.L. have provided services under the Better Access programme.
Both authors are on the board of the Australian Psychological Society.
Funding
The author(s) received no financial support for the research, authorship and/ or publication of this article.
References
Crump C, Sundquist K, Sundquist J, et al. (2014) Sociodemographic, psychiatric and somatic risk factors for suicide: A Swedish national cohort study. Psychological Medicine 44: 279–289.
Harvey SB, Deady M, Wang MJ, et al. (2017) Is the prevalence of mental illness increasing in Australia? Evidence from national health surveys and administrative data, 2001–2014. Medical Journal of Australia 206: 490–493.
Jorm AF (2018) Australia’s ‘Better Access’ scheme: Has it had an impact on population mental health? Australian and New Zealand Journal of Psychiatry 52: 1057–1062.
Lincoln TM, Jung E, Wiesjahn M, et al. (2016) What is the minimal dose of cognitive behavior therapy for psychosis? An approximation using repeated assessments over 45 sessions. European Psychiatry 38: 31–39.
Whiteford HA, Buckingham WJ, Harris MG, et al. (2014) Estimating treatment rates for mental disorders in Australia. Australian Health Review 38: 80–85.
Published in Australian and New Zealand Journal of Psychiatry 2019
Thank you for this important contribution to the literature in this area. Can I clarify something ? You note that K10 scores continued to show a decline even when the number of sessions was reduced from 18 to 10. My eyeballing of your very helpful table it that K10 scores began to trend up in 2014 and I would be very interested to see the data for 2017. Perhaps I have misunderstood your table ? If so, could you please advise.
Hi Lisa, thanks for reading and taking an interest.
The initial analysis done showed an overall downward trend over the time period in question, but remember this is a main effect and main effects often hide interesting comparisons. Your observation that things got worse after 2011 is almost certainly true, although not as bad as things were in 2004.
The 2017 data should be interesting.