A number of my GP colleagues have reached out to me in the past few days asking what they can do to manage the waves of anxious people experiencing Coronavirus related anxiety and panic. This anxiety is stretching already-precious staff resources as well as producing some very aggressive behaviour directed toward staff. I have written this with GPs in mind in the hope that a few of these ideas are helpful.
Learn to know the difference between health anxiety as a disorder vs a description.
Health anxiety or hypochondriasis is a real psychological condition and is one of the complex anxiety disorders (along with OCD, GAP and PTSD). For these patients, they live their entire lives with the belief that either they already have a terminal illness that no one is taking seriously, or that they are developing a terminal illness. These patients present with the following symptoms
- They are incredibly health focussed and are vigilant for any change in their body that may indicate illness
- They typically spend a lot of time reading up on their symptoms which further terrifies them of how bad it is
- They often seek excessive assays, scans and physicals and importantly are not reassured by the results
- They often spend lots of time “checking”, they poke that funny looking mole until it bleeds, or palpate that odd lump until it is inflamed, and these checking behaviours often worsen the clinical picture and reinforce for them the seriousness of their illness.
For these people, the current sentiment around COVID-19 is an absolute nightmare, and many of them are not doing well at all. Having just spent several sleepless months worrying about PM 2.5 related respiratory illness relating to the bushfires, they are on the alert for any sign of respiratory distress. Now being told that there is a virus spreading where a minor respiratory illness can turn fatal is absolutely terrifying for them.
For this group of patients, the most helpful thing you can do right now is to check in with them about their symptoms, make sure they are doing ok. They are at risk of calling several times a day looking for reassurance during this particular crisis. If they have not ever had psychological treatment for their health anxiety, maybe this is the time to consider a psychological or psychiatric referral. This disorder is treatable with varying degrees of success. Even if they have not found treatment helpful, supportive counselling can be considered to at least look after them during this unfolding crisis.
Anxiety as a contagion
Anxiety is just as contagious as COVID-19, in fact, thanks to social media, one anxious person can now ‘infect’ more people than ever before. There is a reason it’s a bad idea to yell “Fire!!” in a crowded theatre. This contagion effect was clearly illustrated last week by the nationwide run on toilet paper and to a lesser extent, biscuits. Interestingly, non-perishable foodstuffs remained largely unaffected.
For GP practices, this anxiety contagion can be an incredible drain. People who have never travelled overseas, have no known contact with infected people but who have a runny nose are demanding COVID-19 testing. As you are all aware, the PPE requirements, survey, differential diagnosis interview, and possible swab process are massively time-consuming. Many practices would do little else if they tested everyone who wanted to “be better safe than sorry”. GPs must continue to tend to other patients whilst also managing the current risk.
For this type of anxiety, the best cure is information.
The government has been wrong-footed by the speed of this outbreak, different states are issuing different advice, and the messaging from the federal government has been unclear at best, and downright confusing at worst. Coupled with the fact that the situation is evolving and therefore so is the advice, there is not currently a clear message getting through as to what sensible people should do (other than washing your hands, which despite its effectiveness doesn’t quite feel like one is doing enough). In this Infomation vacuum, people are doing what the last ten years have taught them to do when they want to know something; google it.
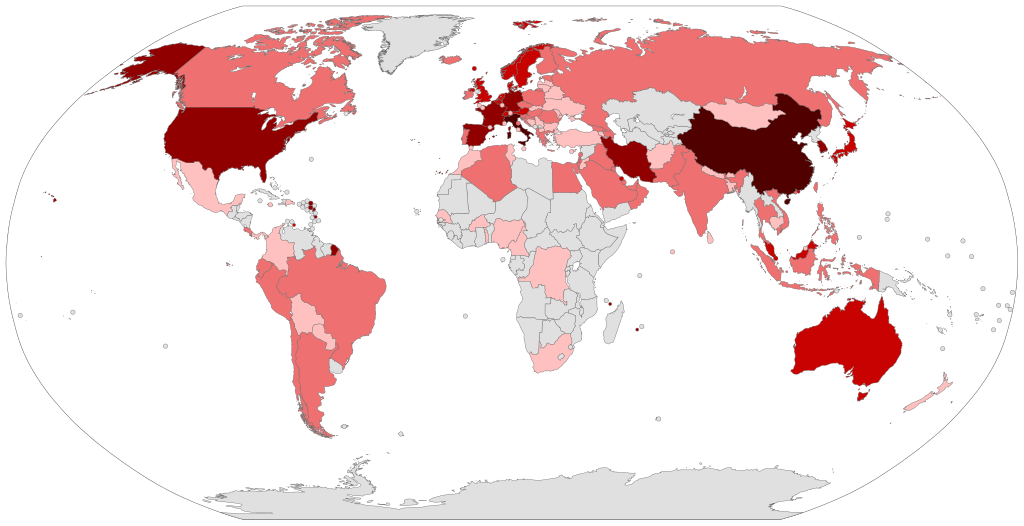
Google is of course filled with horror stories from Hubei province and Northern Italy and Iran. These accounts tell of medical systems beyond the brink of collapse, of having to triage the limited number of ventilators, of medical staff dying of illness and of post-apocalyptic scenes of suffering. If this is what awaits Australia in a few weeks time, then the toilet paper hoarders suddenly aren’t looking so silly.
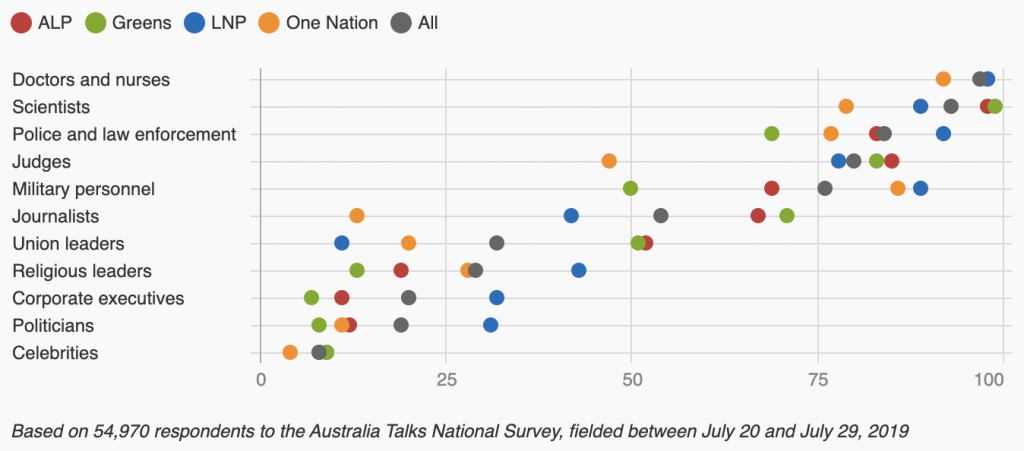
What is needed is a counter-narrative and it must come from local GPs. Recent research tells us that Doctors and nurses remain the most trusted professional in Australia (97%), while politicians are trusted by 20% of the population.
https://www.abc.net.au/news/2019-11-27/the-professions-australians-trust-the-most/11725448
I have been so impressed with the number of GP practices who are engaging with social media (some for the first time) to try and get clear information out to people. The Public wants to know what the truth is, they want to know what they can do to help both themselves and their community, and they want to know as the situation eases or deteriorates.
When people wake up in the morning, they don’t need to read the clickbait headlines to articles hidden behind paywalls and they don’t want to sift through 20 pages of dry information from the health department. They want a daily update;
- Is the situation in my city worse than it was yesterday?
- How about our area are there any active alerts or closures?
- If I’ve got a sore throat can I go to work or should I stay home?
- What are the reasons id call up and arrange to be tested?
No one will thank you for doing the job of the media and the politicians, but no one else is going to do it. Remember, as a GP, you are probably the most trusted person several thousand people in your neighbourhood know. If you tell them the facts they will listen.